(GS2: Mechanisms, Laws, Institutions, and Bodies constituted for the Protection and Betterment of these Vulnerable Sections.)
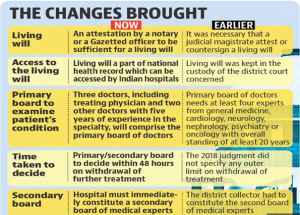
A five-judge SC bench decided to modify the existing rules for “living wills” as established in its 2018 decision allowing passive euthanasia, in order to make the process of passive euthanasia easier.
Living will is a person’s right to make an advance directive about the course of his or her treatment, including the removal of life support, if such a situation arises.
Evolution of the concept of ‘Living Will’ in India:
- Law Commission of India (2006) in its 196th Report: A patient’s decision to not receive medical treatment did not constitute an attempt to commit suicide under Section 309 IPC. Also, a doctor who obeys the instructions of a competent patient to withhold/withdraw medical treatment does not commit a breach of professional duty.
- Aruna Shanbaug case (2011): The SC allowed passive euthanasia for the nurse lying in a vegetative state at a hospital in Mumbai.
- Puttaswamy case/ the Right to Privacy case (2017): – Article 21 includes the concept of individual dignity and thus allows passive euthanasia.
- Common Cause case (2018): The SC decided that passive euthanasia will be legally allowed henceforth in India and also laid down guidelines for living wills.
The term “euthanasia” is derived from Greek, literally meaning “good death”. Taken in its common usage, however, euthanasia refers to the termination of a person’s life, to end their suffering, usually from an incurable or terminal condition. It is for this reason that euthanasia was also coined the name “mercy killing”.
| For:
Rights-based argument: it is argued that as part of our human rights, there is a right to make our own decisions and a right to a dignified death. Beneficence: Advocates of euthanasia express the view that the fundamental moral values of society, compassion and mercy, require that no patient be allowed to suffer unbearably, and mercy killing should be permissible. The difference between active euthanasia and passive euthanasia: Supporters of euthanasia claim that active euthanasia is not morally worse than passive euthanasia – the withdrawal or withholding of medical treatments that result in a patient’s death. In line with this view, it is argued that active euthanasia should be permitted just as passive euthanasia is allowed |
| Against:
The sanctity of life:Religious proponents argue that “it is the sole prerogative of God to bestow life and to cause death. Euthanasia as murder: Society views an action which has a primary intention of killing another person as inherently wrong, in spite of the patient’s consent Abuse of autonomy and human rights: It has also been argued that patients’ requests for euthanasia are rarely autonomous, as most terminally ill patients may not be of a sound or rational mind. The role of palliative care: It is often argued that pain and suffering experienced by patients can be relieved by administering appropriate palliative care, making euthanasia a futile measure The rights of vulnerable patients: If euthanasia were to become an accepted practice, it may give rise to situations that undermine the rights of vulnerable patients. The doctor-patient relationship and the physician’s role: Active voluntary euthanasia and physician-assisted suicide undermine the doctor-patient relationship, destroying the trust and confidence built in such a relationship. |
